‘Today is day 353’: Woman takes 189 pills a week nearly 1 year after COVID-19 diagnosis to combat symptoms
PORTLAND, Ore. - Amy Watson, a preschool teacher who lives in Portland, Oregon spoke with FOX TV Stations in June detailing some of the long-term symptoms she has dealt with since contracting COVID-19 in April of last year.
"Today is day 93," said Watson in June. She shared a photograph of her thermometer, which read 100.3 on June 18, 2020. She first tested positive for COVID-19 on April 11, 2020, after falling ill with flu-like symptoms in mid-March of last year.
On March 3, 2021, nearly a year after she first experienced flu-like symptoms, her thermometer reads 100.7.
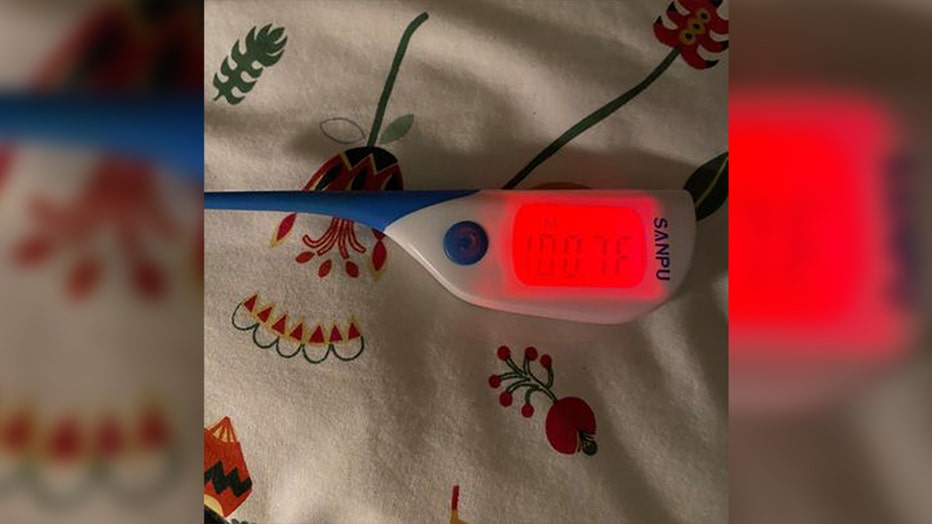
Screenshot of Amy Watson’s temperature taken on Mar., 3.
"Today is 353," said Watson on March 3 as she approaches one year since she first fell ill. "I pretty much wake up nauseous every morning," Watson said.
She says she takes 189 pills, capsules and tablets every week to help quell an array of symptoms that have plagued her life over the past year.
March 15 will mark one year since she first came down with flu-like symptoms.
On Sept. 15 of 2020, Watson posted an update on her condition on Facebook, writing, "Six months. 185 days. I still have a fever."
"I also have a diagnosis: post-viral dysautonomia. My autonomic nervous system (ANS) was damaged by COVID-19. This controls things like breathing, heart function, digestion, perspiration, temperature regulation, and vision. I have brain damage," Watson wrote, including a flurry of other long-term and devastating symptoms.
Some other symptoms she described roughly nine months ago included constant fever, burning sensations on her skin and severe fatigue.
Watson says she has experienced new issues since then, although she says some things are "a little better" thanks to medication she has been prescribed. Hypertension and chronic migraines are among the new symptoms she’s experienced since her last interview with FOX TV Stations.
She calls them, tongue in cheek, "post COVID gifts."
A long list of COVID-19 complications
"One of the unexpected gifts that COVID has brought is at my seven-month mark, a whole bunch of GI [gastrointestinal] symptoms and I won’t get into that but I have some procedures scheduled in the near future to try to sort that out," Watson said. "Some things have gotten better, some things have gotten worse."
Watson takes a stimulant for her incessant fatigue, but she says many of her symptoms have remained the same since she first fell ill.
She describes having tachycardia episodes that she hasn’t been tested for yet, but says the erratic fluctuation in her heart rate has been consistent. Watson uses an Apple Watch to measure her heart rate and says simple tasks like showering will trigger a worrisome heart rate elevation.
Dr. Mady Hornig, an immunologist and professor of epidemiology at Columbia University, was researching the long-term effects of a viral infection like COVID-19 when she spoke with FOX TV Stations in June.
RELATED: Medical imaging shows the true scope of long-term effects caused by COVID-19
Hornig had also been dealing with tachycardia episodes ever since she began to experience COVID-19 symptoms herself in April of 2020, which she said continued to impact her daily life for several months.
Tachycardia is a condition that can make your heart beat abnormally fast, reducing blood flow to the rest of your body, according to The Mayo Clinic.
On June 22, Hornig said her pulse registered at 135 beats per minute, which she said occurred just from her sitting at her computer. She said a normal pulse for someone her age would be around 60-70 beats per minute.
Watson, meanwhile, says her temperature is still elevated every day, and most days climbs past 100 or 101 degrees.
She recently received an invitation by the National Institutes of Health to participate in a neurological study. Watson will travel to the NIH’s headquarters in Bethesda, Maryland with hopes of finding a light at the end of a long and arduous tunnel of illness.
According to the NIH, the study will examine people with long-term symptoms in hopes of identifying the changes in the nervous system to better understand how the disease impacts the body.
‘Long COVID’ and the complexity of coronavirus symptoms
During the onset of the pandemic, many doctors were baffled by some of the deleterious effects caused by COVID-19 — originally thought to be just a respiratory illness.
But cases like Watson’s and thousands of others illustrate that the effects of the novel coronavirus can be much more complicated.
Radiological images recently published at Northwestern University detailed the various types of long-term effects of COVID-19 including rheumatoid arthritis flares, autoimmune myositis or "COVID toes," and more.
In a study published on Feb. 17 in the journal Skeletal Radiology, the collections of images included ultrasounds, x-rays, MRIs, and CT scans which confirmed and illustrated the causes of various COVID-19 symptoms.
"We’ve realized that the COVID virus can trigger the body to attack itself in different ways, which may lead to rheumatological issues that require lifelong management," said corresponding author Dr. Swati Deshmukh.
Currently, several symptoms of COVID-19 identified in the study are not recognized by the U.S. Centers for Disease Control and Prevention. Symptoms like "COVID toes" and "rheumatoid arthritis" aren’t listed on the CDC’s website detailing long-term effects of the coronavirus.
According to the CDC, the most commonly reported long-term symptoms include:
- Fatigue
- Shortness of breath
- Cough
- Joint pain
- Chest pain
Other reported long-term symptoms include:
- Difficulty with thinking and concentration (sometimes referred to as "brain fog")
- Depression
- Muscle pain
- Headache
- Intermittent fever
- Fast-beating or pounding heart (also known as heart palpitations)
More serious long-term complications appear to be less common but have been reported. These have been noted to affect different organ systems in the body. These include:
- Cardiovascular: inflammation of the heart muscle
- Respiratory: lung function abnormalities
- Renal: acute kidney injury
- Dermatologic: rash, hair loss
- Neurological: smell and taste problems, sleep issues, difficulty with concentration, memory problems
- Psychiatric: depression, anxiety, changes in mood
The CDC said, "While most persons with COVID-19 recover and return to normal health, some patients can have symptoms that can last for weeks or even months after recovery from acute illness."
According to a study from the NIH, researchers found evidence to suggest that brain damage may be a product of COVID-19. Researchers uncovered blood vessel damage and inflammation in the brains of 19 deceased COVID-19 patients.
"We found that the brains of patients who contract infection from SARS-CoV-2 may be susceptible to microvascular blood vessel damage. Our results suggest that this may be caused by the body’s inflammatory response to the virus" said Dr. Avindra Nath, clinical director at the NIH’s National Institute of Neurological Disorders and Stroke (NINDS).
Nath, the senior author of the study, added that while COVID-19 is most commonly known to be a respiratory illness, he hopes this study will help the medical community recognize the scope of complications that can arise out of contracting the deadly coronavirus.
‘No, you are not crazy. You are not alone.’
Because of the complexities of the virus, Watson and many other "long haul survivors" are confused and frustrated. Health care providers who have treated them have been left with their hands in the air after lingering symptoms did not seem to subside.
In some instances, Watson said her health care providers expressed disbelief that the novel coronavirus could cause many of symptoms she has been experiencing for nearly a year.
That was why she started her own Facebook group as a means to support other "long haulers" who have felt isolated by their symptoms due to the lack of understanding and available treatment by the medical community.
She says there are roughly 14,000 members from more than 100 countries and says multiple groups have been created depending on the onset of people’s illness.
A screenshot of one of the many Facebook support groups for COVID "long haulers" created by Amy Watson.
"Welcome. No, you are not crazy. You are not alone," reads a title page for one of the Facebook groups she’s created.
Watson says she now feels more validated, although it doesn’t make up for all the denial she and many others faced early on. She says she remains in close contact with many of the members of the long-haul Facebook groups — they’re like family, she says.
"It was my partner’s suggestion to create it because I just felt so lonely and isolated and confused, and when I got my diagnosis, I asked the doctor, ‘like OK now what?’ and he was like, ‘survive! just keep doing it. You’re surviving,’ so that wasn’t exactly what I was asking," Watson said.
The cost of long-term COVID-19
Watson expressed gratitude that she was able to receive a positive COVID-19 test, which allowed her to qualify to be covered for treatment for the coronavirus under provisions of the CARES Act. The $2 trillion legislation that was signed into law on March 27 allocated $175 billion in relief funds to health care providers to ensure that patients would not be sent "surprise medical bills" after being treated for COVID-19.
RELATED: The cost of COVID-19: Amid illness, Americans face heavy financial burden in testing and treatment
Watson said because of this, her medical expenses have been manageable, but others have not been so lucky.
The HRSA Covid-19 Claims Reimbursement program provides claims reimbursement to health care providers who are providing treatment for uninsured individuals. But the program will only provide reimbursement when "COVID-19 is the primary reason for treatment," a spokesperson said.
Potentially devastating out-of-pocket coronavirus expenses, for some, don’t end with testing and treatment.
Hanna Lockman, a Louisville, Kentucky resident, first noticed her coronavirus-like symptoms in March of 2020 and has experienced lasting negative effects to her health ever since — and the bills kept piling up.
Speaking with FOX TV Stations in July, Lockman said she had been hospitalized three times, racking up 13 emergency room visits over the course of her illness, eventually maxing out her deductible in May.
"I just calculated the cost of my charges so far and the total – if I didn’t have insurance — would be over $180,000," she said. "I maxed out my insurance for the year around the first week of May, so thankfully everything since then has been covered at 100%. However, maxing out my insurance means spending $7,900."
Lockman was a member of one of Watson’s Facebook support groups for COVID-19 "long haulers."
Lockman said the disease hit her like a ton of bricks, and while her initial fears brought her to conclude that she had come down with the flu, she tested negative for that, eventually leading doctors to treat her for pneumonia, which she had never contracted before.
Considering the timing of her illness, she was convinced it was COVID-19, and despite asking to be tested, she said doctors refused.
Lockman said she pressed her doctors for a coronavirus test and was continuously told no. "I thought I was crazy," she said. "There is a pandemic going on and you will not test me for a pandemic virus."
"It was a very weird feeling being refused a test and having to fight with doctors. I’ve never had that experience," Lockman recalled.
Lockman eventually received a test three weeks after her symptoms first began, which came back negative. Lockman added that her doctor said the test was most likely a "false negative."
But according to Lockman, all that mattered to her insurance company was the negative result, which rendered her ineligible for benefits under the CARES act and unable to be covered for any treatments related to the coronavirus. This, despite there being multiple reports and documented cases of faulty testing in the United States.
On July 8, The U.S. Food and Drug Administration issued a warning letter for clinical labs and health care providers over COVID-19 tests manufactured by global medical technology company Becton, Dickinson and Company (BD) which has produced coronavirus tests the department says are at high risk for false positive results.
In a study conducted by the company and cited by the FDA, approximately 3% of results from tests using the BD SARS-CoV-2 Reagents for the BD Max System were false positives.
Living as a COVID-19 ‘long-hauler’
Among the things Watson listed that have kept her morale up throughout her physically and emotionally taxing experience are the validation of thousands of other COVID-19 "long haulers," the love and support from her family, and the companionship of her pets.
Her two Whippets, Ollie and Maple, and her two preschool class guinea pigs have been a source of comfort for her in her time of need. "They’re great company, they’ve been so great to have to hug and lean on," Watson said, referring to her dogs.
But the biggest relief of all has been receiving the validation she and many other long haulers sought for an entire year.
Watson noted recent recognition of long-term COVID-19 illness from Dr. Anthony Fauci, the nation’s leading expert on infectious diseases.
Last month, the Associated Press reported that the NIH is launching research to understand the causes and consequences of the lingering brain fog, breathing problems and malaise reported by many recovering COVID-19 patients.
Fauci said some studies have shown up to 30% of patients report symptoms that can endure for months, complicating their return to normal routines and work, and plunging many recovering patients into depression.
Fauci noted at a White House coronavirus briefing on Feb. 24 that work at the NIH had begun thanks to more than $1 billion provided by Congress for COVID-related medical research. Government scientists are looking to enlist doctors and research institutions around the country in the effort to learn about "long-haul" COVID-19.
The Associated Press contributed to this story. This story was reported from Los Angeles.

